Psychology of Survival: Mastering Mindset and Stress Management
What would you do if panic hit at home and your plan vanished in a moment?
You need clear steps that keep your family steady when alarm rises. This guide turns complex brain facts into easy actions you can use today.
Survival mode triggers the amygdala, floods cortisol, and can make sleep, food, and hydration fall away. That state drains health and focus fast.
We show simple tools—CBT moves, grounding, STOP, TIPP, and the Dive Response—that help you reset before choices slip. Expect family templates, drills, and routines that fit real life.
Plan with care, practice with your household, and return here for updates. This living guide centers on your safety, decision supports, and when to seek professional help.
Key Takeaways
- You’ll get a family-focused roadmap to steady decisions under pressure.
- Short, skills-based tools help lower arousal and restore clear thinking.
- Ready-to-use templates and drills make preparedness practical at home.
- Learn to spot survival mode early and use simple resets like grounding.
- Know when at-home steps suffice and when to reach professional care.
Why Mindset Matters in Survival: Proper Planning Starts in Your Head
Your best defenses start not with gear but with clear, practiced plans that a tired brain can follow.
The planning-consideration loop: think, test, adjust
Use a simple cycle: plan, try it under low pressure, note what worked, then refine. Repeat until steps are automatic.
Quick template: Goal → Risks → Resources → First three actions → Stop rule → Debrief.
- Write decisions for common scenarios to create a prefrontal assist.
- Practice short loops so the sequence sticks even when your state shifts.
- Keep three-step checklists and color codes for kids.
Individual vs. family mindset: aligning needs and roles
Map each person’s needs to roles: meds, mobility, food, pet care. Assign alternates and post roles where everyone sees them.
“Plans that live on paper free your thinking when seconds count.”
| Role | Main tasks | Alternate |
|---|---|---|
| Lead communicator | Contact, updates, radios | Spouse/neighbor |
| Logistics | Grab gear, route check | Teen/neighbor |
| Care & comfort | Kids, meds, snacks | Grandparent/partner |
Bookmark this guide and run seasonal drills. Over time your ability to act calmly and your family’s responses will improve.
The Science of Survival Mode: Brain, Body, and the Fight-or-Flight Response
When danger feels close, your brain reroutes priorities so survival actions outrank planning.
What this looks like inside you: the amygdala ramps up vigilance while the prefrontal cortex quiets. That swap makes complex thinking harder and speeds simple reactions.
Amygdala vs. prefrontal cortex: how stress hijacks thinking
The amygdala shouts “urgent” and pushes quick action. Your planner—the prefrontal cortex—loses horsepower.
That means decisions you normally make in minutes may take longer or feel fuzzy. Notice when you struggle to choose words, follow steps, or keep a plan on track.
Cortisol, heart rate, and what your body is telling you
Cortisol helps mobilize energy, but high levels over time harm sleep, mood, and overall health. Watch for rising heart rate, shallow breathing, clenched muscles, and tunnel vision.
These symptoms are signs you can act on. Use a two-minute body scan to decide the best reset tool: breathing for fast heart rate, cold water for surging impulses, or movement for restlessness.
- Simple map: amygdala = urgent; prefrontal = planner.
- Track tells: shaking hands, word-finding issues, irritability.
- Log episodes: time, trigger, body signals, tool used, outcome.
“Your body is working to protect you; with the right tools, you can bring your thinking mind back online.”
Psychology of Survival: Mindset and Stress Management Under Crisis
Acute events and long stretches of worry both push your brain into a narrow, protective state.
You and your family need simple ways to spot what’s happening in real time. Watch for quick spikes that last minutes to hours and for low-grade strain that stretches weeks or months.
Real-time checklist for symptoms: overwhelm, narrowed focus, skipped meals, poor sleep, irritability, constant scanning. Use this to decide: rest, grounding, or help.
Trauma, pandemics, and prolonged high alert
Past trauma or a recent pandemic can keep your nervous system ready long after danger fades. That prolonged mode raises anxiety and wears down coping skills.
When a survival mode isn’t laziness
Replace blame with accuracy: this mode prioritizes immediate needs at the cost of long-term tasks. Teach your household simple phrases like “pause and breathe” to trigger role switches.
- Map weekly triggers and energy crashes.
- Install short grounding breaks: breath, water, sunlight.
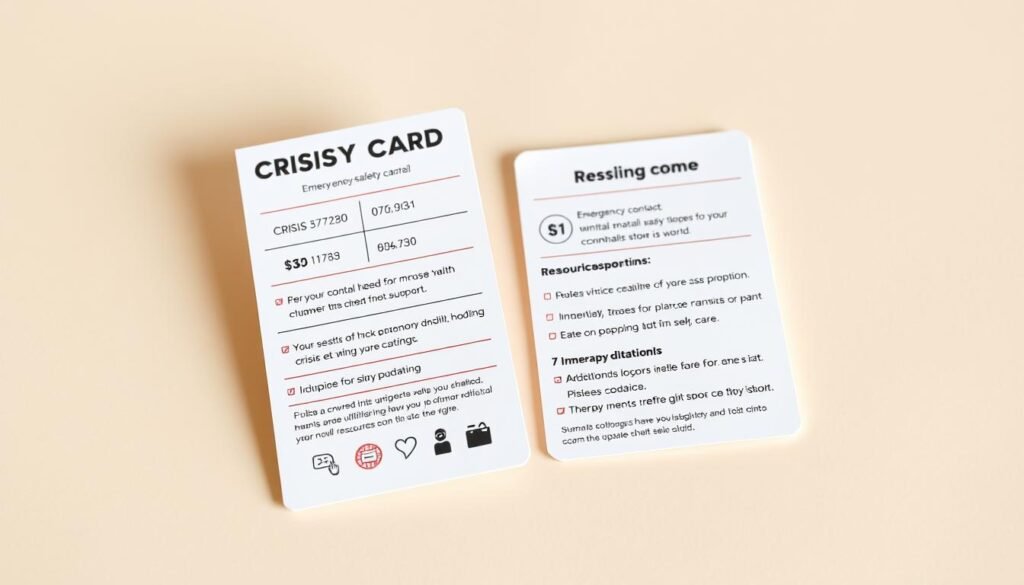
- Create a pocket “first-aid for stress” card with three steps: breathe, temperature shift, move.
“Name what you see, act with tiny steps, and plan an exit to professional care if symptoms persist.”
Bookmark this evolving guide and review your family’s plan regularly so small fixes become automatic before a crisis grows.
Real-Life Impacts: Focus, Decisions, and Daily Tasks When You’re Overwhelmed
When your brain narrows, basic chores slip and choices feel heavy.
Decision fatigue shows up as a steady lack of focus. You skip meals, forget water, skip exercise, and lose sleep. These gaps hurt your health and make the next task harder.
Decision fatigue and missed basics
Watch for when every small way feels draining. That is a cue to simplify the day.
- Use a Daily Basics checklist for your household: drink water on waking, eat simple meals, move, and set a lights-out window.
- Batch choices: pre-plan snacks, lay out clothes, and set reminders for meds and hydration.
- Break large tasks into one-step actions so momentum builds and overwhelm fades.
Micro-habits that stabilize your day
Add tiny, real-life habits that stick. These take little time but pay off in focus.
| Habit | Cue | Quick action |
|---|---|---|
| Hydration | Wake-up | 5 sips of water before coffee |
| Movement | After bathroom | 10 squats |
| Reset | Before email | 60-second paced breathing |
| Sleep prep | One hour before bed | Dim lights, stretch, no screens |
Family planning matters: pair habits with everyday cues like school drop-off or dinner. Use visible trackers for kids so the household supports each other.
“Keep a ‘when stuck’ card: 3 deep breaths, drink water, stand up, pick one tiny step.”
Bookmark this blog for updates and review your 24-hour self-care plan as a family each week.
Immediate Crisis Tools: How to De-escalate Your Stress Response Fast
Quick, practiced moves can stop a spike in arousal so you act with purpose rather than panic.
STOP skill: pause, notice, then act
STOP is short and repeatable: Stop. Take a step back. Observe sensations and surroundings. Proceed mindfully toward your goal.
- Print a pocket STOP card for each family member.
- Practice STOP at low-stakes moments (spilled milk, noise) so it becomes automatic when emotions rise.
TIPP: rapid shifts that change your body
Use TIPP to flip physiological arousal and get clearer thinking.
- Temperature: ice pack to cheeks or a hot shower to interrupt escalation.
- Intense exercise: 30–90 seconds (jumping jacks, stairs) to burn off adrenaline.
- Paced breathing: inhale ~5s, exhale ~7s with belly rise for 1–3 minutes.
- Paired muscle tension: clench on inhale, release on exhale across shoulders to legs to ease pain and tension.
Dive response: a fast, safe reset
The dive response uses cold water to slow heart rate and redirect blood flow to the core. Submerge your face for about 15 seconds when impulses feel dangerous.
- Create a “calm kit”: ice packs, a timer, a towel, printed steps, and grounding objects.
- Teach kids an easy script: “Cold‑Move‑Breathe” for quick recall.
“Practice these tools together so your household’s responses are steady when a real crisis arrives.”
If anyone faces a medical or psychiatric emergency, call 911 or go to the nearest emergency room immediately.
Staying Goal-Directed Under Pressure: Pros & Cons and ACCEPTS Distractions
High-pressure moments test your priorities, but clear rules help you act with purpose.
Prep a simple pros & cons sheet for your top triggers. Write the impulse, the pros and cons of acting, and the pros and cons of waiting. Finish with a short pre-commitment line you can read fast when time is tight.
How to build your quick pros & cons
Keep three sheets: one for each major trigger. Put copies on your phone and in your wallet so you can reference them when modes shift.
- Impulse: name it in one line.
- Acting: list 2 pros and 2 cons.
- Not acting: list 2 pros and 2 cons.
- Pre-commit: one sentence you will follow.
ACCEPTS: a quick menu to interrupt racing thoughts
When your thoughts speed up, pick one ACCEPTS item and do a short task for two minutes. This gives your mind space and lowers reactivity.
- Activities: walk a block, read a page, or do a quick puzzle.
- Contributing: text support to a friend or tidy one shelf.
- Comparisons: recall a harder time you handled well.
- Emotions: watch a short funny clip to shift feelings.
- Pushing away: jot worries in a “later list” or a worry box.
- Thoughts: count objects of a color or recite lyrics to anchor attention.
- Sensations: hold a textured object and note five details.
Print or save templates for both the pros & cons sheet and the ACCEPTS menu. Keep them with your first-aid for stress card and review them with your household. For an additional printable worksheet, see the crisis survival skills handout.
“Pre-commitment shortens the time you need to decide and protects your goals when emotions rise.”
Family Playbook: Templates, Drills, and Routines That Keep Everyone Calm
When the household feels stretched, small prepared steps help everyone stay steady.
Use a clear Family Stress Plan that lists Roles (primary/backup), Signals (for example, “I need a pause”), Safe Words (like “Blue”), and Meeting Points for home and away.
Family stress plan template: roles, signals, and safe words
Add each person’s personal needs: meds, mobility aids, sensory tools, pet care, and hydration reminders so essentials aren’t missed.
Breathing and grounding routines for kids, teens, and adults
- Kids: 3-2-1 grounding — 3 things you see, 2 you feel, 1 you hear (under a minute).
- Teens: 60-second box breathing (4-4-4-4) plus a two-minute music break.
- Adults: paced 5-7 breathing for deeper calm; pair with a quick posture shift to reset the mind.
Weekly check-in script: feelings, needs, tasks
Try this short script in 10–15 minutes: “One feeling I had this week,” “One need I have now,” “One task I’ll take,” and “One way we can help.” Start with water for everyone and end with one appreciation per person.
Home practice drills: short, fun, repeatable
- Lights-out drill: 5 minutes of flashlight practice and calm-voice roles — keep it playful.
- Rotate drill leaders so kids gain confidence; celebrate small wins to reinforce participation.
- Post routines on the fridge and tuck copies in go-bags. Revisit the playbook monthly to swap what didn’t work and keep what did.
“This playbook gives you a simple way to keep relationships steady when survival mode hits.”
Relationships in Survival Mode: Communicating Needs Without Escalation
High arousal can make you short with loved ones, even when you mean well. That shift can strain relationships fast. Use clear scripts so you don’t add guilt to the load.
Be honest, set boundaries, seek support. Tell others your current state, name what you need, and offer a simple next step.
Be honest and use short scripts
- I statement: “I’m feeling flooded and need five minutes to breathe so I can talk clearly.”
- Boundary: “I can’t discuss solutions right now; I can listen for 10 minutes at 7 p.m. Can we pause until then?”
- Ask for help: “I need help with dinner tonight; could you chop veggies while I finish this call?”
- For kids: “My brain is in fast mode. Let’s do three breaths together, then I’ll answer your question.”
Repair, timing, and lowering anxiety
Agree on brief repair phrases ahead of time like “Can we restart?” or “Same team?” Use a house rule: no problem-solving when someone is flooded. Pick a calmer time in your weekly check-in to revisit tough topics.
“Mirror and label feelings: ‘You sound worried about tomorrow; did I get that right?'”
End talks with a clear next step — who does what, and by when — so the conversation leads to action, not a loop of worry. Keep this page bookmarked for new scripts and tools your family can try.
When to Get Professional Help: Therapy, Triage, and Safety
Knowing when a problem needs professional care is as essential as any first-aid kit.
Consider therapy when symptoms persist, get worse, or stop you from doing daily tasks. CBT and other skills-based approaches help shift patterns that keep your brain in fight‑or‑flight mode. These methods are effective for trauma, anxiety, and long-term health impacts.
CBT and skills-based approaches
CBT teaches specific steps you can practice daily. DBT‑informed tools build in-the-moment regulation and goal-directed behavior. Set follow-up checkpoints with your clinician to adjust plans as your journey progresses.
Build a 24-hour self-care plan and crisis safety card
Draft a simple daily plan: sleep window, meals/hydration, movement blocks, social check-ins, and calm routines. Add early warning signs and first-line tools (paced breathing, cold water, intense exercise).
“Planning when you’re well makes it easier to get the right help fast when you need it.”
| Item | What to list | Why it matters |
|---|---|---|
| Emergency info | Name, DOB, meds, allergies | Speeds care in hospital |
| Contacts | Clinician, 2 trusted people | Who to call if you need support |
| Warning signs | Key symptoms, pain spikes | Triggers earlier help |
| Coping steps | STOP, TIPP, Dive Response | Immediate tools to reduce arousal |
| Transport plan | Preferred facility, when to call 911 | Clear actions for loved ones |
Keep copies of the safety card at home, in your go‑bag, and share with trusted supporters. If travel or timing is hard, use telehealth—continuity matters more than perfection. For clinical resources on skills-based care, see this peer-reviewed summary.
Conclusion
Good planning shortens decision time and protects what matters most when seconds count.
You now have science-backed tools, family templates, and simple drills to guide your household through high-pressure moments. Keep basics—water, food, sleep, movement—visible so the body and mind recover faster. Use quick resets like STOP, TIPP, and the Dive Response when emotions surge, then return to goal tools such as Pros & Cons and ACCEPTS.
Revisit your playbook monthly, print a crisis safety card, and share this guide with everyone in your home. If problems grow or last, seek professional help such as CBT to speed recovery in mental health. Bookmark this page and return often; this journey builds steady ways to protect your life, roles, and state when it matters most.
FAQ
What is the main idea behind mastering mindset and stress when facing danger?
You learn to shape your thinking so you act clearly under pressure. That means simple plans, rehearsed routines, and short mental checks that keep your choices practical. Practice reduces panic and helps your body follow your calm lead.
How do I create a planning loop that actually works in real situations?
Use a cycle: think through options, test them quickly, then adjust based on results. Keep tests small and low risk. Repeat this loop often so it becomes automatic when time is tight. That steady rhythm lowers anxiety and boosts confidence.
How do you balance individual needs with family roles during an emergency?
Talk ahead about strengths and tasks. Assign clear roles—who handles kids, supplies, navigation, or first aid. Keep roles flexible so people can step in if someone is overwhelmed. Regular drills make role shifts less stressful.
How does stress change the way your brain makes decisions?
High alarm activates quick, gut-level responses and dials down deliberate thinking. The more intense the stress, the more you favor speedy actions over complex problem solving. Training and simple checklists help you recover thoughtful choices fast.
What body signals tell you stress is getting out of hand?
Watch for racing heart, shallow breathing, muscle tension, headaches, and trouble focusing. Early signs let you pause and use calming tools before symptoms worsen into fatigue or chronic strain.
How can I tell the difference between healthy alertness and chronic overwhelm?
Healthy alertness feels focused and time-limited. Chronic overwhelm sap energy, disrupts sleep, and makes daily tasks hard. If stress lasts weeks or harms relationships, it’s a sign to change habits or seek help.
What simple habits stop decision fatigue from derailing basics like food, sleep, and exercise?
Automate essentials: set meal plans, fixed sleep times, and short daily movement. Use checklists for supplies and prioritize one restorative habit each day. Tiny wins keep momentum and prevent burnout.
What is the STOP skill and how do I use it when panic rises?
STOP means Stop, Take a breath, Observe what’s happening, and Proceed with a plan. It gives you a brief reset to slow the stress cycle and choose a safer, calmer action.
How does the TIPP method calm you quickly and when should you use it?
TIPP combines temperature shifts, brief intense exercise, paced breathing, and muscle tension to shift your nervous system fast. Use it when you feel overwhelmed and need a short, effective reset before making decisions.
Can cold water really help during a panic episode?
Yes. A cold splash or holding something cold can trigger a dive reflex that slows heart rate and brings down acute arousal. It’s a quick tool to regain control when you feel flooded by fear.
How do pros and cons lists help when pressure makes choices hard?
They force you to slow down and see trade-offs. Keep lists short and practical—two to three key points each. That clarity cuts through rush and reduces regret later.
What does ACCEPTS stand for and how does it stop racing thoughts?
ACCEPTS is a set of distraction techniques—Activities, Contributing, Comparing, Emotions, Pushing away, Thoughts, Sensations. Use one or two to shift attention and lower distress so you can respond more clearly.
What should a family stress plan include to keep everyone calm?
Include roles, a short list of supplies, simple signals or safe words, and meeting points. Add regular drills and a basic communication tree. Clear, practiced steps cut confusion when seconds count.
How do I teach kids and teens breathing or grounding routines?
Keep methods short and playful—counted breaths, balloon breaths, or five-finger grounding. Practice during calm times so kids know the routine when upset. Make it part of daily family rhythm.
What does a weekly check-in with family look like?
Ask three quick questions: How are you feeling? What do you need? What small task can we do this week? Keep it under 10 minutes to stay consistent and useful.
How do short home drills make a real difference?
Brief, fun repetitions build muscle memory for responses and reduce fear. When practice is normal, real events feel more manageable. Aim for five-minute drills that you repeat weekly.
How can you ask for help from a partner without starting an argument?
Use clear, calm language: name what you need, explain how it helps, and offer a small role. For example: “I feel overwhelmed. Can you handle food and kids for 20 minutes while I check supplies?” This reduces defensiveness.
When should you consider professional help for trauma or prolonged stress?
If sleep, daily function, or relationships decline for weeks, or if you have intense flashbacks or self-harm thoughts, contact a licensed therapist or crisis services. Early support speeds recovery and keeps you safe.
What therapies work best for skills-based stress and trauma care?
Treatments like cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT) teach practical skills for emotional regulation, distress tolerance, and problem solving. Look for clinicians who offer structured skill training.
How do you build a 24-hour self-care plan and crisis safety card?
List one priority for morning, one for afternoon, and one for evening—small acts that restore you. On a crisis card, note your triggers, coping steps, emergency contacts, and next actions. Keep it accessible and brief.


